Overview
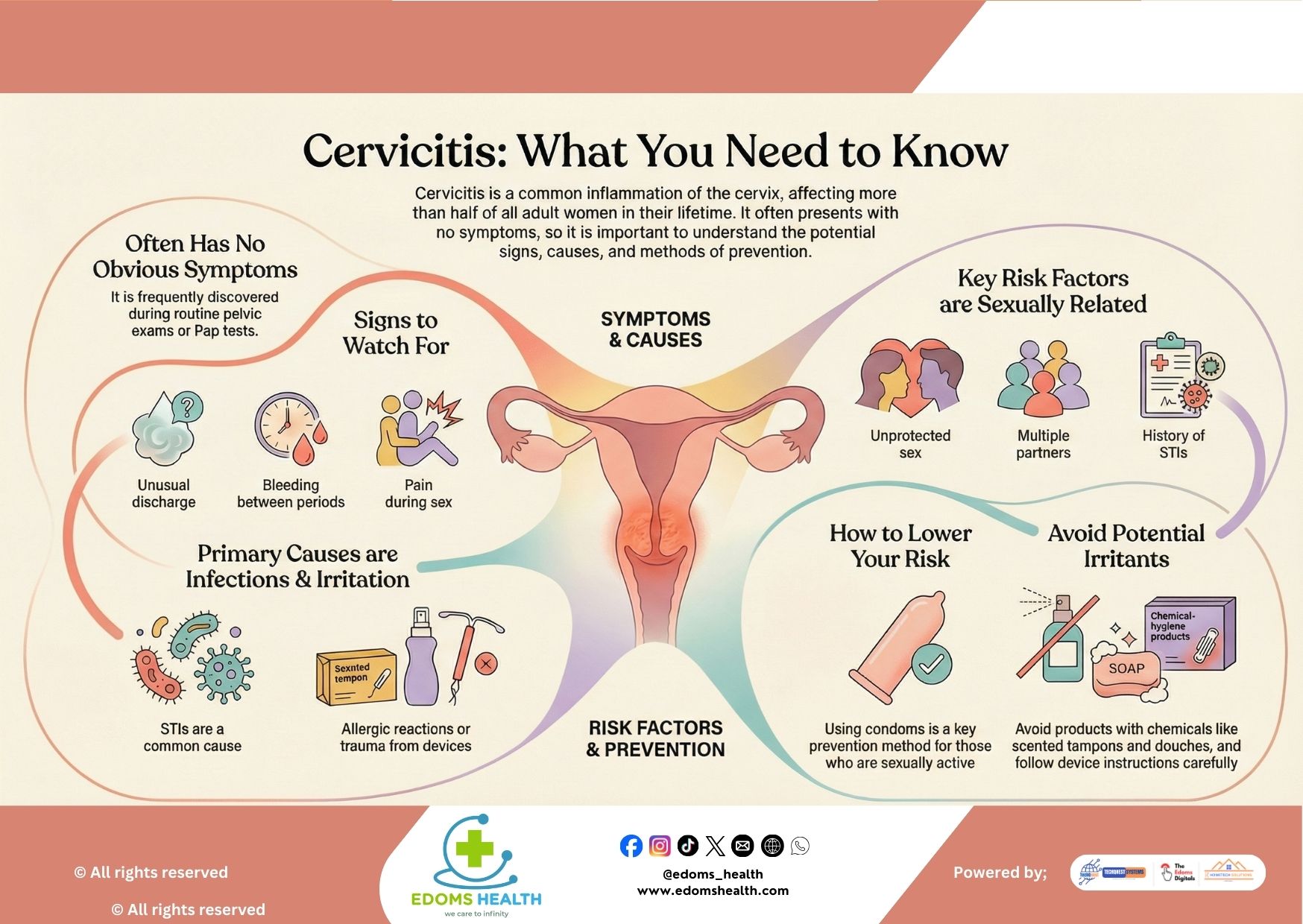
Cervicitis is an inflammation of the cervix—the narrow, lower part of the uterus that opens into the vagina. While often mild and treatable, it can sometimes lead to more serious health concerns if left unaddressed. Because cervicitis frequently presents without obvious symptoms, awareness and regular gynecological care are essential for early detection and treatment.
Symptoms and Causes: What to Watch For
Often Has No Obvious Symptoms
One of the challenges with cervicitis is that it can be asymptomatic—meaning you might not notice anything unusual. It’s often discovered incidentally during a routine pelvic exam or Pap smear. However, when symptoms do occur, they may include:
- Abnormal vaginal discharge, which may be yellow, gray, or green and sometimes foul-smelling
- Vaginal bleeding between periods or after intercourse
- Pain during sex (dyspareunia)
- A feeling of pelvic pressure or discomfort
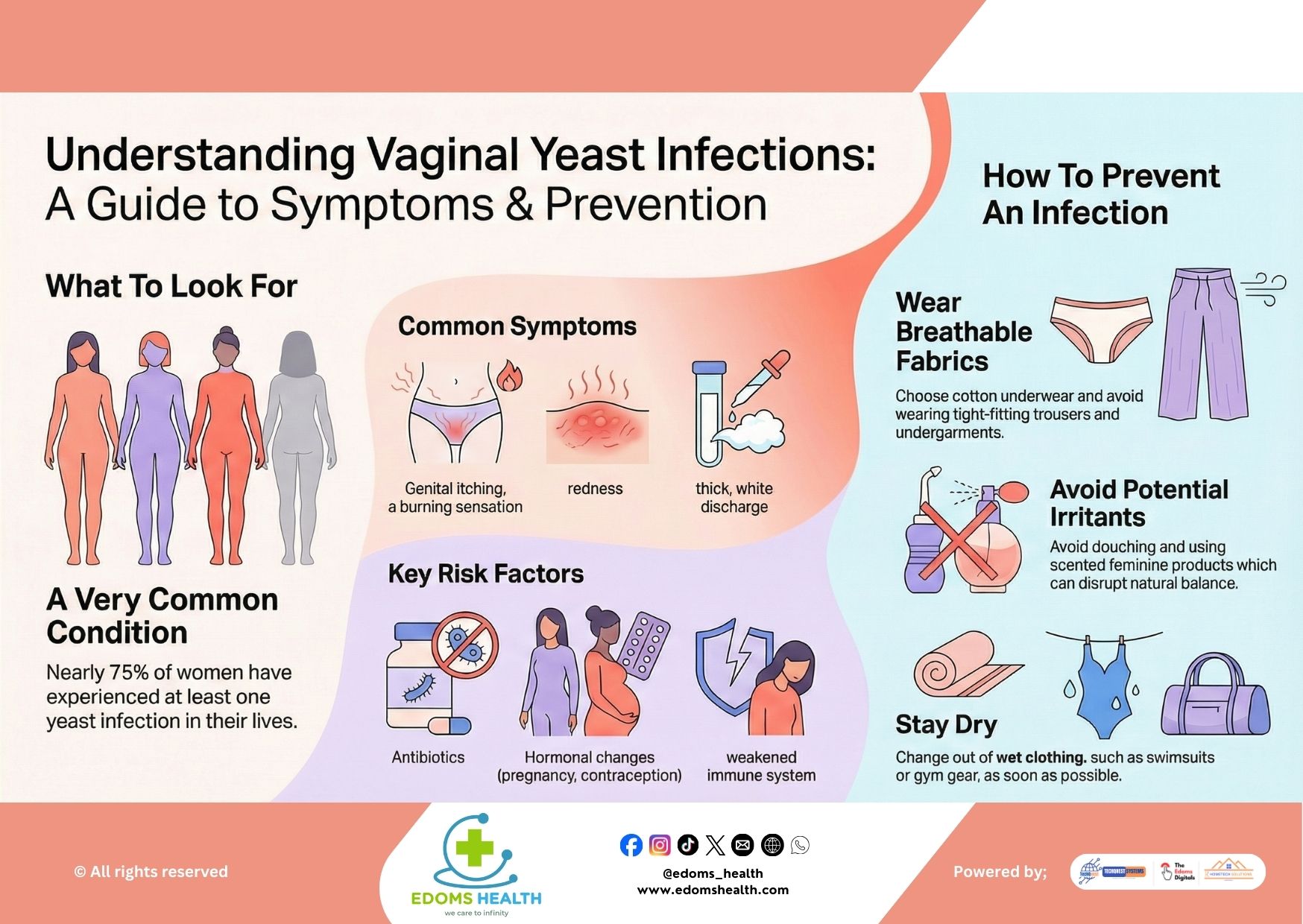
- Vaginal itching or irritation
- Frequent or painful urination in some cases
Primary Causes: Infections and Irritation
Cervicitis can result from both infectious and non-infectious causes:
Infectious Causes:
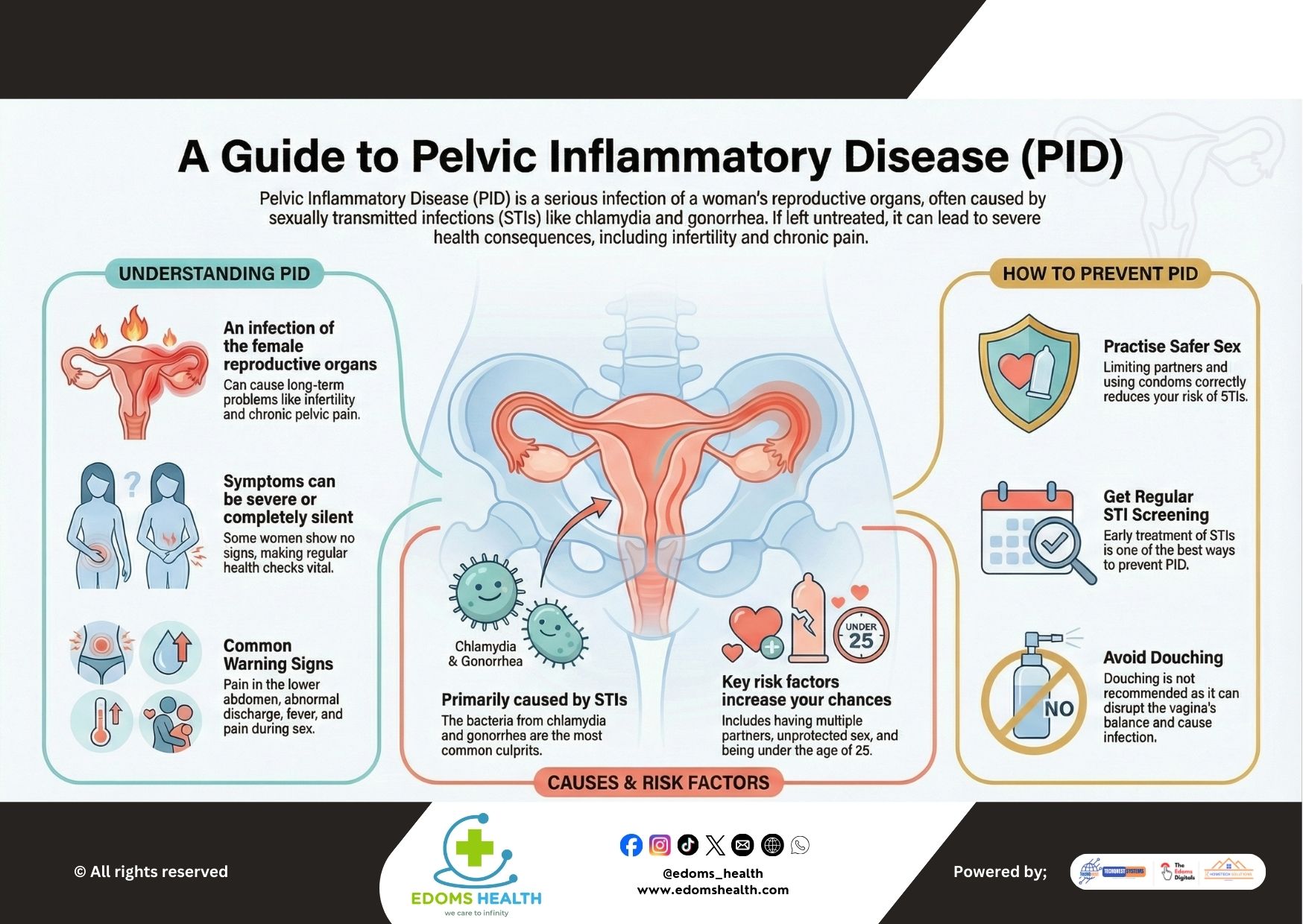
- Sexually Transmitted Infections (STIs): The most common infectious causes include chlamydia, gonorrhea, trichomoniasis, and genital herpes.
- Bacterial Vaginosis: An imbalance of vaginal bacteria can contribute to cervical inflammation.
- Other Infections: Less commonly, other bacterial or viral infections may be involved.
Non-Infectious Causes:
- Chemical or Physical Irritants: Exposure to products such as scented tampons, douches, vaginal deodorants, spermicides, or latex (in condoms) can irritate the cervix.
- Medical Devices: The use of intrauterine devices (IUDs) or diaphragms, particularly if not inserted correctly or if hygiene isn’t maintained.
- Allergic Reactions: Sensitivity to materials in contraceptives or hygiene products.
- Hormonal Imbalances: Fluctuations in estrogen levels, particularly during perimenopause or menopause, can thin cervical tissue and increase susceptibility to inflammation.
Risk Factors and Prevention
Key Risk Factors Are Sexually Related
Since many cases of cervicitis are linked to sexually transmitted infections, certain behaviors and histories can increase your risk:
- Having multiple sexual partners
- Engaging in unprotected sex
- A history of STIs
- Starting sexual activity at an early age
- Having a partner with an STI or multiple partners
How to Lower Your Risk
Preventing cervicitis involves reducing exposure to both infectious and irritant causes:
- Practice Safe Sex: Use condoms consistently and correctly to reduce the risk of STIs.
- Limit Sexual Partners: Reducing the number of sexual partners can lower your exposure to STIs.
- Get Regular Screenings: Routine STI testing and Pap smears help detect infections and inflammation early, even without symptoms.
- Avoid Potential Irritants: Steer clear of scented tampons, douches, vaginal sprays, and other products that contain harsh chemicals. Always follow instructions for medical devices like IUDs and diaphragms.
- Maintain Good Hygiene: Gentle cleansing with mild, unscented soap and water is sufficient—avoid internal washing or douching, which can disrupt natural flora and cause irritation.
- Communicate with Partners: Open, honest conversations about sexual health and STI testing with your partner(s) are important for mutual protection.
Diagnosis and Treatment
If cervicitis is suspected, your healthcare provider may perform:
- A pelvic exam to visually assess the cervix
- A Pap test or swab to collect cervical cells for analysis
- STI testing through urine samples or swabs
Treatment depends on the underlying cause:
- For bacterial STIs: Antibiotics are prescribed, and it’s important that sexual partners are treated simultaneously to prevent reinfection.
- For viral infections (like herpes): Antiviral medications may be recommended.
- For non-infectious causes: Removing the irritant (e.g., discontinuing a certain product) and allowing time for healing is often sufficient. In some persistent cases, minor procedures like cryotherapy or laser treatment may be considered.
Why Timely Care Matters
Left untreated, cervicitis can lead to complications such as:
- Pelvic inflammatory disease (PID)
- Chronic pelvic pain
- Increased risk of HIV transmission
- Fertility issues or ectopic pregnancy
- Pregnancy-related complications
Take Charge of Your Cervical Health
Cervicitis is common and manageable, especially when identified early. By understanding the signs, minimizing risk factors, and staying proactive with regular gynecological care, you can protect your reproductive health and overall well-being.
If you experience any symptoms of cervicitis or are due for a pelvic exam or STI screening, schedule an appointment with your healthcare provider. Early attention can prevent complications and support long-term health.