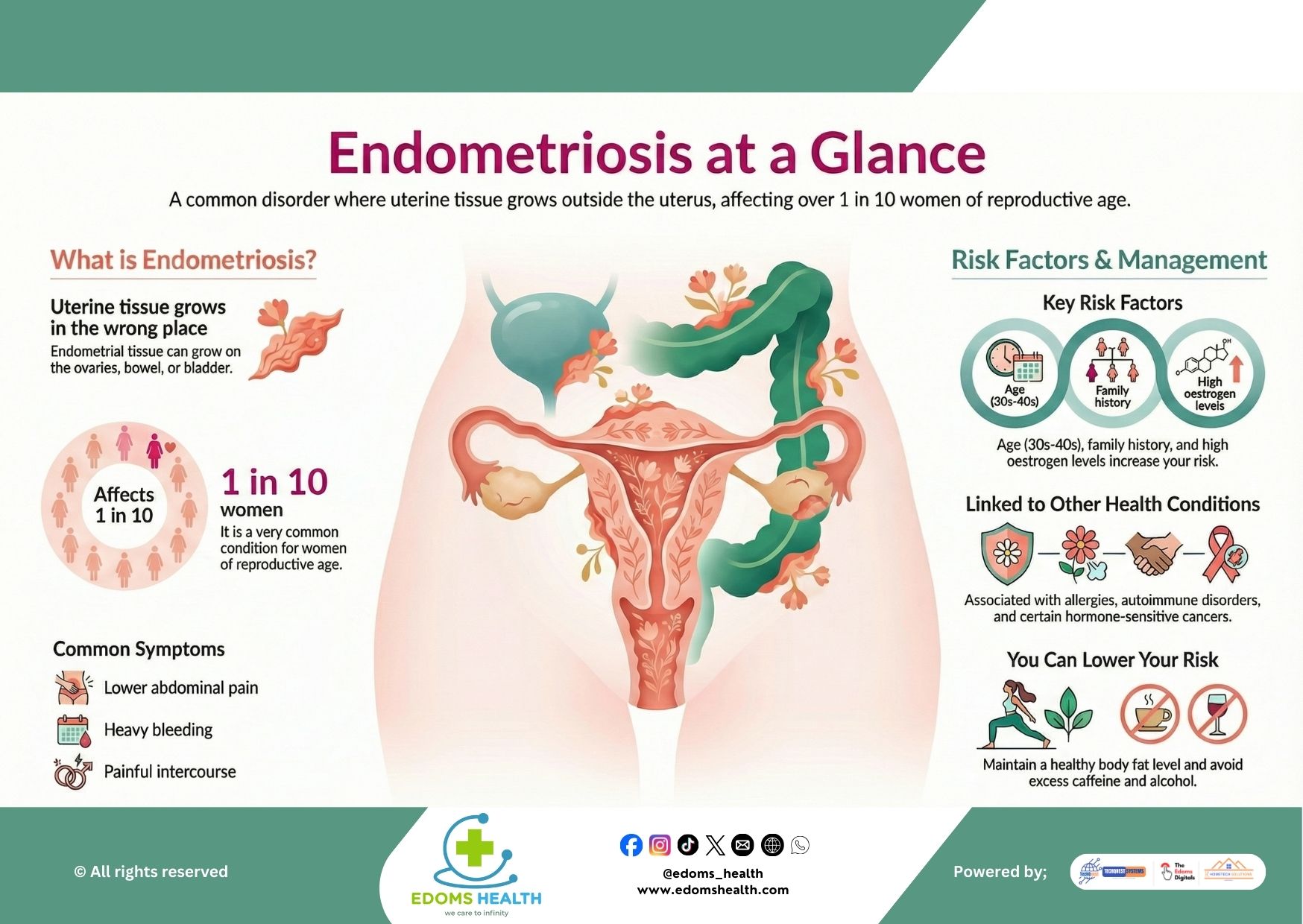
Endometriosis is a common but often misunderstood gynecological disorder that affects more than 1 in 10 women of reproductive age worldwide. Despite its prevalence, many people go undiagnosed for years, facing chronic pain and significant impacts on their quality of life. By increasing awareness and understanding, we can support earlier diagnosis, better management, and improved well-being for those affected.
What Is Endometriosis?
Endometriosis occurs when tissue similar to the lining of the uterus (endometrium) grows outside of the uterus. This tissue can implant on organs such as the ovaries, fallopian tubes, bowel, bladder, and pelvic lining. Like the uterine lining, this tissue thickens, breaks down, and bleeds with each menstrual cycle. However, because it has no way to exit the body, it becomes trapped, leading to inflammation, scarring, adhesions, and chronic pain.
A Widespread but Underdiagnosed Condition
- Affects approximately 190 million women and girls globally.
- Despite being common, diagnosis is often delayed by 7–10 years on average due to normalized symptoms and lack of awareness.
Common Symptoms
Endometriosis symptoms can vary widely but often include:
- Severe menstrual cramps (dysmenorrhea)
- Chronic pelvic pain outside of menstruation
- Heavy or irregular bleeding
- Pain during or after intercourse (dyspareunia)
- Pain with bowel movements or urination, especially during periods
- Fatigue, bloating, and nausea
- Difficulty getting pregnant (infertility or subfertility)
It’s important to note that pain levels do not necessarily correlate with the extent of the condition—some with mild endometriosis experience severe pain, while others with advanced disease may have few symptoms.
Risk Factors
While the exact cause of endometriosis is still not fully understood, several factors may increase risk:
- Age: Most commonly diagnosed in women in their 30s and 40s, though symptoms often start earlier.
- Family History: Having a mother, sister, or daughter with endometriosis increases your risk.
- Reproductive History: Never giving birth, early menarche, or late menopause may be associated.
- High Oestrogen Levels: Hormonal imbalances that increase estrogen exposure.
- Other Health Conditions: Linked to higher rates of allergies, autoimmune disorders, asthma, and certain hormone-sensitive cancers.
How to Lower Your Risk and Manage Symptoms
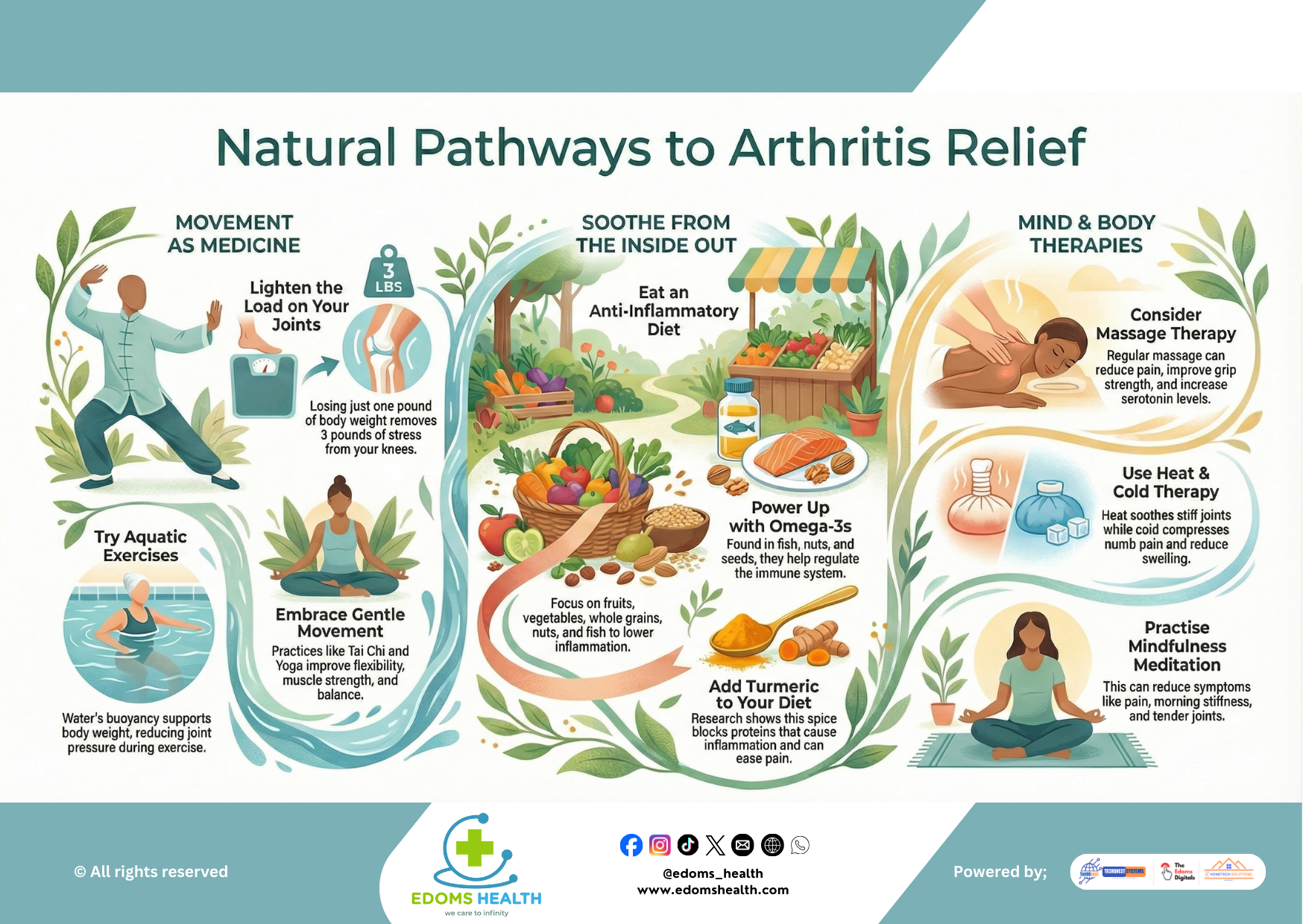
While endometriosis cannot always be prevented, certain lifestyle choices may help reduce risk or ease symptoms:
- Maintain a Healthy Body Weight: Excess body fat can increase estrogen levels.
- Limit Caffeine and Alcohol: Both may influence hormone levels and inflammation.
- Regular Exercise: Can help regulate hormones and reduce pain.
- Balanced Diet: Anti-inflammatory foods (omega-3s, fruits, vegetables) may help manage symptoms.
- Stress Management: Chronic stress can worsen inflammation and pain perception.
Diagnosis and Treatment
Diagnosing endometriosis typically involves:
- Detailed medical history and symptom tracking
- Pelvic exam
- Imaging tests (ultrasound or MRI)
- Laparoscopy—a minor surgical procedure—is the gold standard for definitive diagnosis.
Treatment Options:
- Pain Management: Over-the-counter pain relievers (NSAIDs).
- Hormonal Therapies: Birth control pills, progestins, or GnRH agonists to reduce endometrial growth.
- Surgery: Laparoscopic excision or ablation to remove endometrial implants.
- Fertility Support: Assisted reproductive technologies for those trying to conceive.
- Lifestyle and Complementary Therapies: Physical therapy, acupuncture, diet changes, and counseling.
Living with Endometriosis
Endometriosis is a chronic condition, but with proper care, many people manage their symptoms and lead full lives. Advocacy, education, and supportive healthcare are key. If you suspect you may have endometriosis:
- Track your symptoms in a journal or app.
- Talk to a doctor who specializes in endometriosis or pelvic pain.
- Seek support from communities, online groups, or local organizations.
You Are Not Alone
Endometriosis is more than “bad periods”—it’s a real, often debilitating medical condition. By speaking openly, seeking timely care, and advocating for better research and treatment, we can change the narrative around endometriosis and improve lives.
If you experience symptoms of endometriosis, don’t dismiss your pain. Schedule an appointment with a gynecologist to start the conversation about your health.