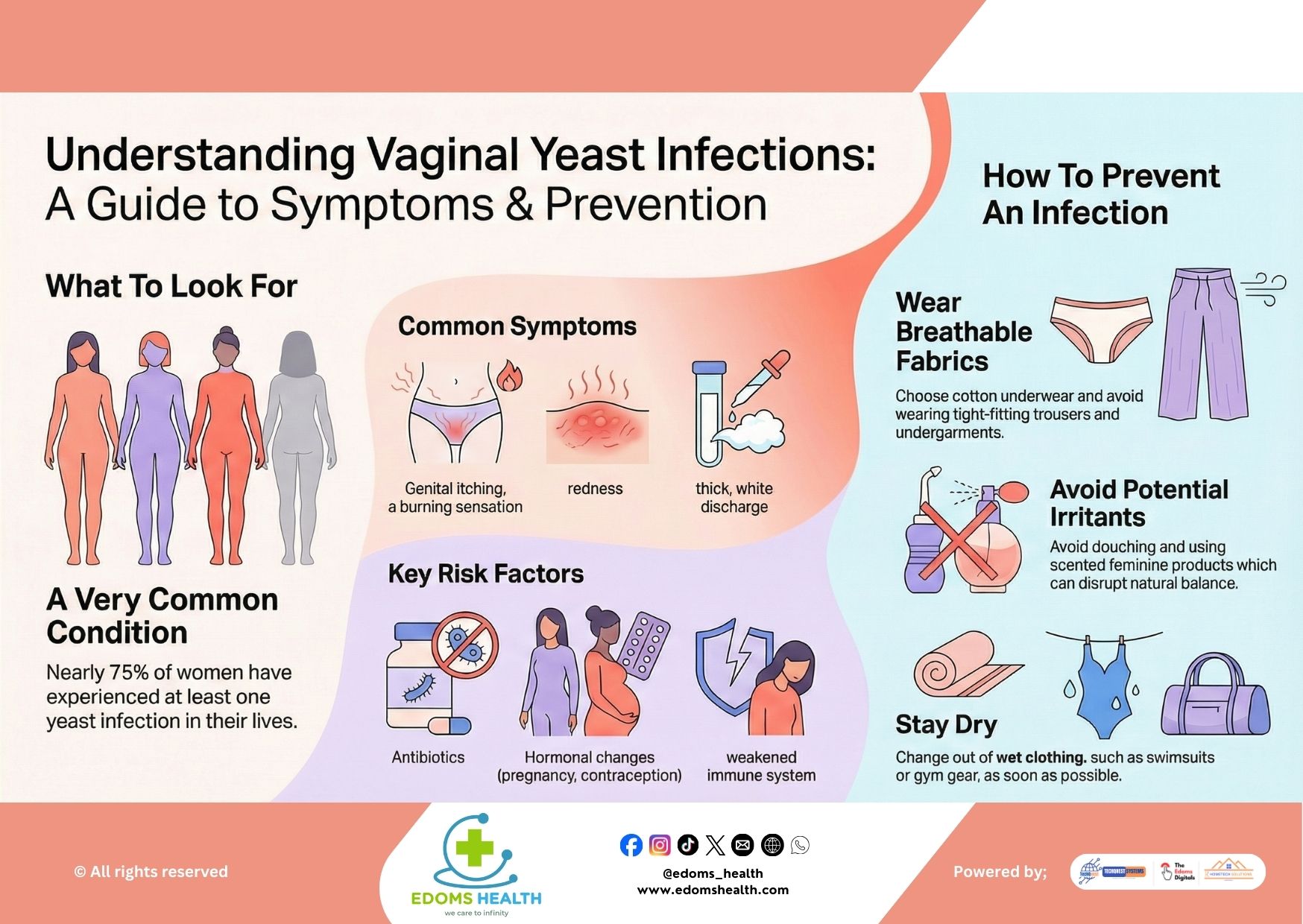
Vaginal yeast infections are one of the most common gynecological issues affecting women, with nearly 75% of women experiencing at least one in their lifetime. Caused by an overgrowth of the fungus Candida albicans, these infections can cause significant discomfort but are typically easy to treat and prevent with the right knowledge and habits. This guide will help you recognize the signs, understand the risk factors, and adopt effective prevention strategies.
What Is a Vaginal Yeast Infection?
A yeast infection occurs when there’s an imbalance in the vaginal microbiome, allowing the naturally occurring yeast Candida to multiply excessively. This overgrowth leads to inflammation and a range of uncomfortable symptoms. While bothersome, yeast infections are generally not serious and respond well to treatment.
Common Symptoms
Yeast infection symptoms can vary from mild to severe and often include:
- Intense genital itching and irritation
- Burning sensation, especially during urination or intercourse
- Redness and swelling of the vulva and vaginal opening
- Thick, white, odorless discharge that resembles cottage cheese
- Vaginal soreness or rash
- Watery vaginal discharge (less common)
If you’re experiencing these symptoms for the first time, or if they persist or worsen, it’s important to see a healthcare provider for an accurate diagnosis, as some symptoms can mimic other conditions like bacterial vaginosis or sexually transmitted infections.
Key Risk Factors
Several factors can disrupt the natural balance of vaginal flora and increase the likelihood of a yeast infection:
- Antibiotic use: Antibiotics can kill beneficial bacteria that keep yeast in check.
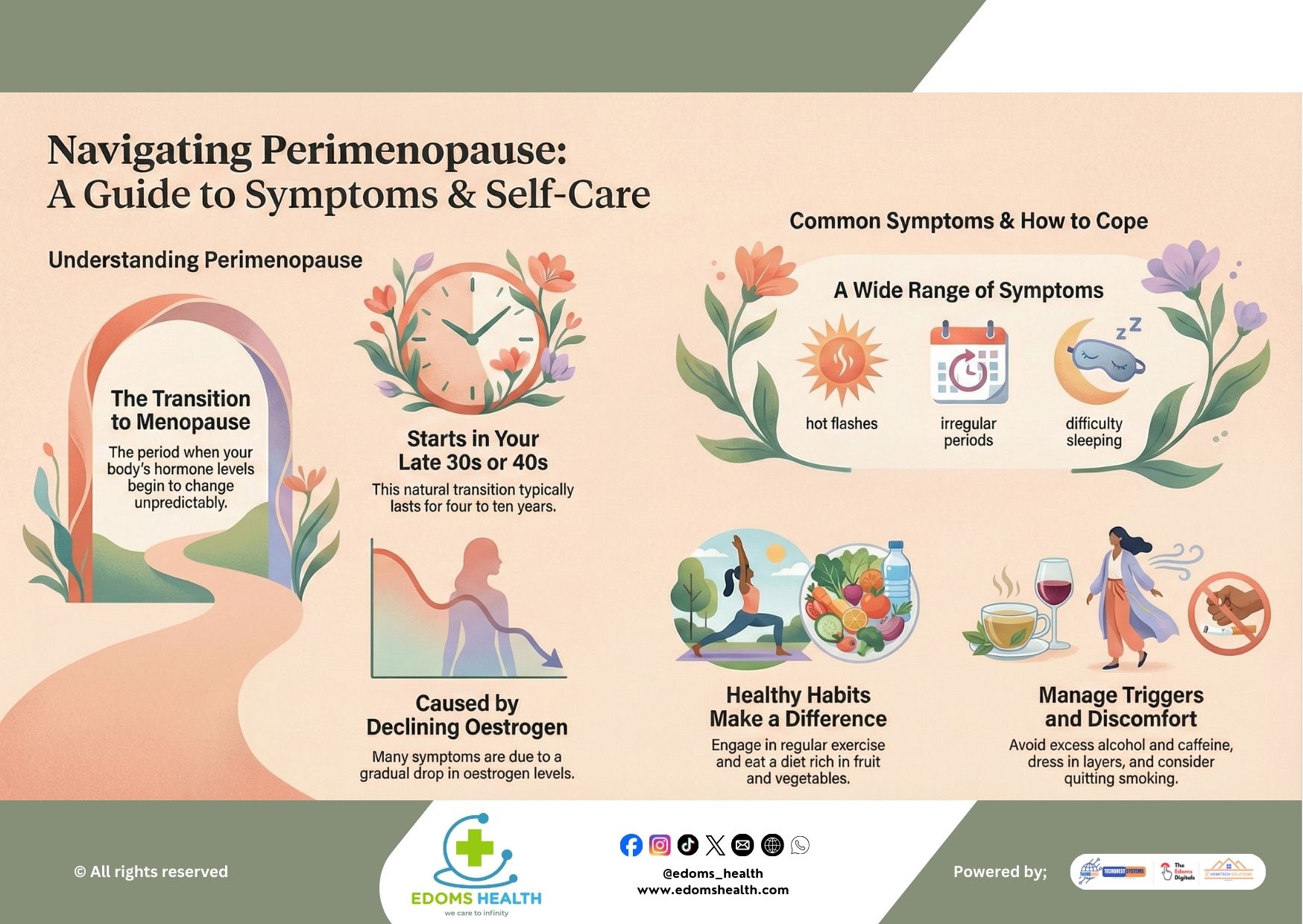
- Hormonal changes: Fluctuations during pregnancy, menopause, or while using hormonal contraceptives can alter vaginal pH.
- Weakened immune system: Conditions such as diabetes, HIV, or stress can make you more susceptible.
- Uncontrolled diabetes: High blood sugar levels can promote yeast growth.
- Poor hygiene habits: Remaining in damp clothing or using irritating products.
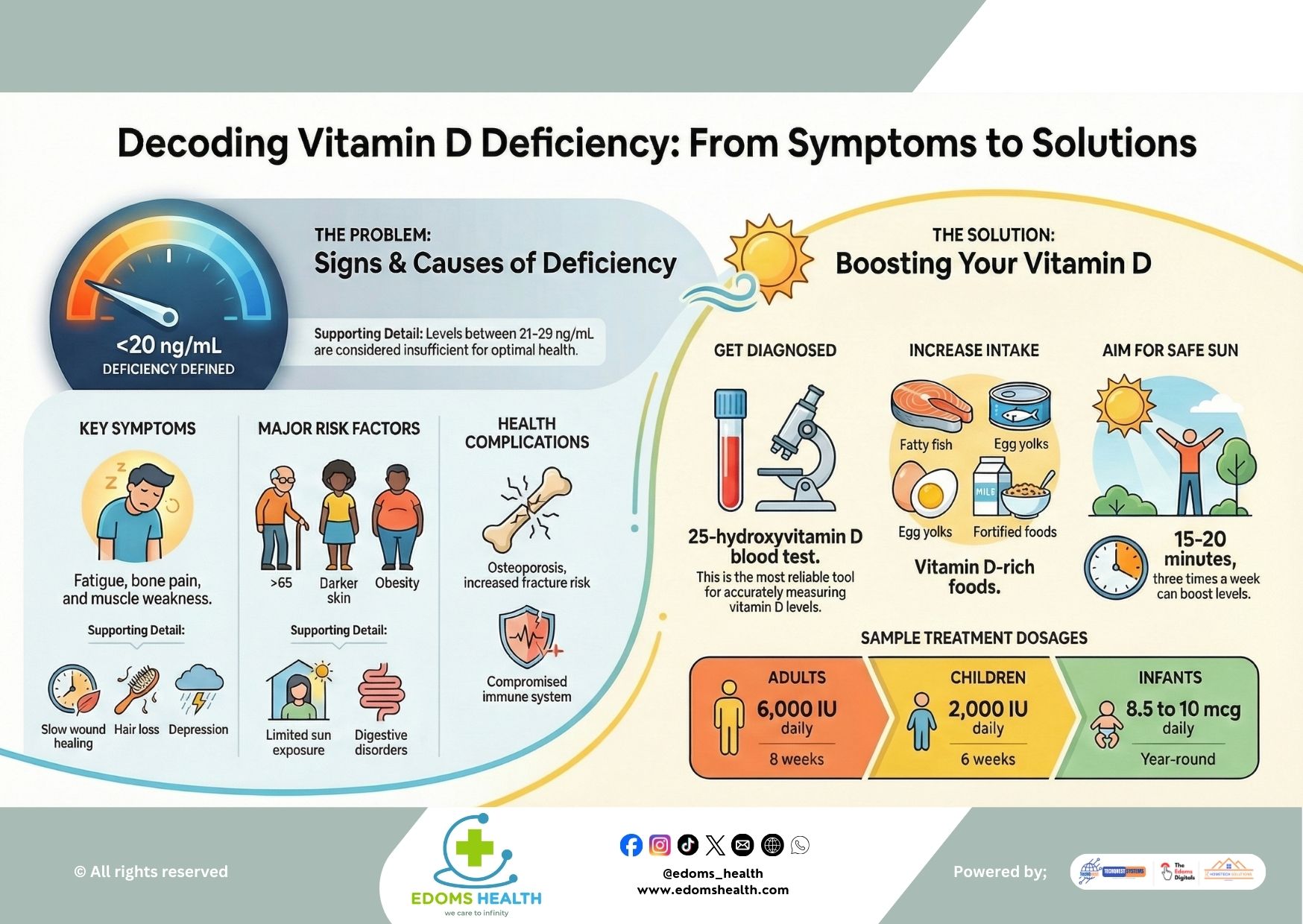
- Diet high in sugar: Yeast thrives on sugar, so a diet rich in refined sugars may contribute to overgrowth.
- Tight, non-breathable clothing: Creates a warm, moist environment ideal for yeast.
How to Prevent an Infection
Preventing yeast infections often comes down to maintaining a healthy vaginal environment and avoiding triggers.
1. Wear Breathable Fabrics
- Choose cotton underwear and avoid synthetic materials that trap moisture.
- Opt for loose-fitting trousers, skirts, and shorts instead of tight jeans or leggings for extended periods.
2. Stay Dry
- Change out of wet clothing—such as swimsuits, sweaty gym wear, or damp underwear—as soon as possible.
- Gently pat the vaginal area dry after bathing instead of rubbing.
3. Avoid Potential Irritants
- Do not douche—it disrupts the natural pH and bacterial balance.
- Avoid scented feminine products including sprays, wipes, bubble baths, and scented tampons or pads.
- Use mild, unscented soap for external cleansing only. The vagina is self-cleaning and does not need internal washing.
4. Practice Healthy Habits
- Wipe from front to back after using the toilet to prevent spreading bacteria from the anus to the vagina.
- Consider probiotics, either through supplements or foods like yogurt with live cultures, to support healthy vaginal flora.
- Manage blood sugar levels if you have diabetes or prediabetes.
- Limit sugar and refined carbohydrate intake.
5. Be Mindful During Antibiotic Use
- If you’re prescribed antibiotics, talk to your doctor about using an antifungal treatment preventively.
- Continue taking probiotics during and after the antibiotic course.
Treatment Options
Most yeast infections can be treated effectively with over-the-counter antifungal creams, ointments, or suppositories (e.g., miconazole, clotrimazole). Oral prescription medication (fluconazole) is also available for more severe or recurrent cases.
When to see a doctor:
- If this is your first suspected yeast infection
- If symptoms don’t improve after using OTC treatments
- If you experience recurrent infections (four or more per year)
- If you’re pregnant, as some treatments are not safe during pregnancy
A Note on Recurrence
Some women experience recurrent yeast infections, which may require longer-term management strategies such as:
- Extended antifungal therapy
- Maintenance doses of medication
- Addressing underlying health issues like diabetes or immune conditions
- Lifestyle and dietary adjustments
You’re Not Alone
Vaginal yeast infections are incredibly common and nothing to be embarrassed about. By understanding the causes and adopting simple preventive measures, you can reduce your risk and maintain better vaginal health. Listen to your body, practice good hygiene, and don’t hesitate to seek medical advice when needed.
If you experience persistent or recurring symptoms, schedule an appointment with your gynecologist or healthcare provider for personalized guidance.
Your comfort and health matter—stay informed, stay proactive, and take gentle care of your body.