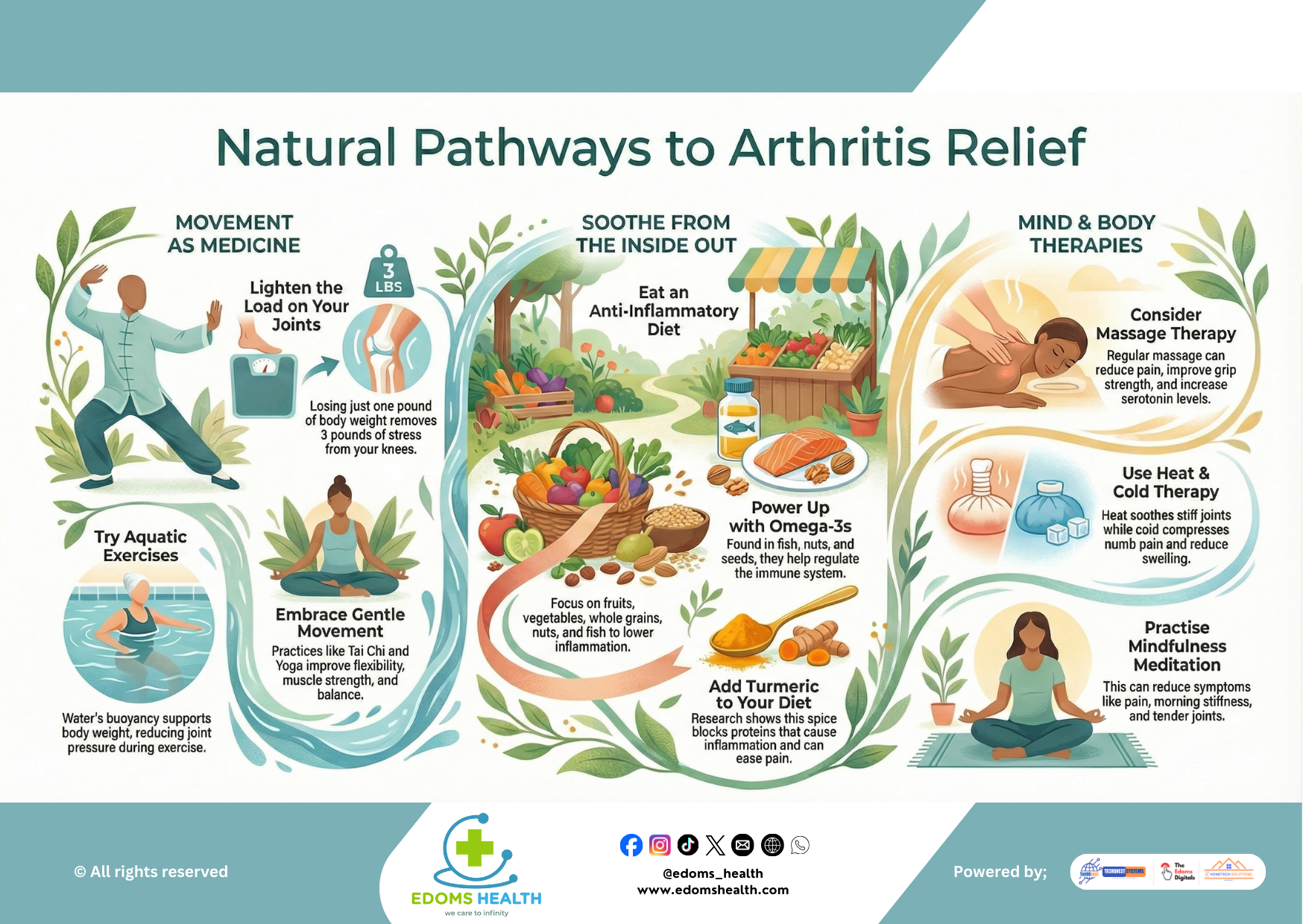
Arthritis, characterized by joint pain, stiffness, and inflammation, affects millions worldwide. While pharmaceutical interventions are crucial for many, a growing body of evidence supports the profound role of natural, integrative approaches in managing symptoms, slowing progression, and enhancing quality of life. This detailed guide explores the multifaceted pathways to arthritis relief, delving into the mechanisms, methods, and practical steps for building a personalized, holistic management plan.
Movement as Medicine – The Biomechanics of Joint Health
Contrary to the instinct to rest painful joints, controlled and appropriate movement is foundational to arthritis management. Inactivity can lead to muscle atrophy, decreased joint lubrication, and increased stiffness.
1.1 The Weight-Joint Stress Equation
The load-bearing joints, particularly the knees and hips, are subject to forces multiples of your body weight during movement.
- The 1:3 Ratio: For every one pound of body weight lost, there is a reduction of three to four pounds of stress on the knees during weight-bearing activities like walking or climbing stairs. This reduction can significantly decrease the rate of cartilage wear and tear and lower pain levels.
- Actionable Strategy: Focus on sustainable weight management through a combination of gentle calorie reduction and low-impact activity, rather than aggressive dieting.
1.2 The Power of Low-Impact and Aquatic Exercise
- Aquatic Therapy: Water provides buoyancy, supporting 90% of your body weight and drastically reducing compressive forces on joints. The water’s viscosity also offers natural resistance for strengthening without weights.
- Recommended Activities: Water walking, Ai Chi (water-based Tai Chi), and shallow-water aerobics. Aim for 45-minute sessions, 2-3 times per week, in warm water (approx. 83-88°F) for optimal muscle relaxation.
- Gentle Land-Based Practices:
- Tai Chi: This ancient martial art emphasizes slow, flowing movements, weight shifting, and mindfulness. Studies show it improves proprioception (joint position sense), balance (reducing fall risk), and lower-body strength, while decreasing pain and stiffness from osteoarthritis.
- Yoga: A well-modified practice enhances flexibility, builds isometric strength (holding poses), and promotes mind-body awareness. Focus on styles like Hatha or Iyengar, using props (blocks, straps) to avoid hyperextension of vulnerable joints.
Nutritional Anti-Inflammatories – The Dietary Foundation
Chronic, low-grade systemic inflammation is a key driver of arthritic pain. An anti-inflammatory diet aims to modulate the body’s inflammatory biochemical pathways.
2.1 Core Principles of the Anti-Inflammatory Diet
Shift from a pro-inflammatory diet (high in processed foods, refined sugars, and certain saturated fats) to one rich in:
- Fruits & Vegetables: High in antioxidants (Vitamins C, E, beta-carotene) and polyphenols that neutralize free radicals and inhibit inflammatory enzymes. Emphasize deeply colored varieties: berries, leafy greens, and cruciferous vegetables.
- Whole Grains: Provide fiber, which is linked to reduced levels of C-reactive protein (CRP), a key marker of inflammation.
- Healthy Fats: The cornerstone of managing inflammation through diet.
2.2 Key Anti-Inflammatory Nutrients & Foods
- Omega-3 Fatty Acids (EPA & DHA):
- Mechanism: They are converted into potent resolvins and protectins in the body, which actively resolve inflammatory processes.
- Top Sources: Fatty fish (wild-caught salmon, mackerel, sardines, herring). Aim for 2-3 servings per week. For plant-based sources (ALA, which the body poorly converts), include flaxseeds, chia seeds, and walnuts.
- Curcumin (from Turmeric):
- Mechanism: A powerful polyphenol that downregulates the NF-kB pathway, a primary signaling molecule that triggers the production of inflammatory cytokines (like TNF-alpha and IL-6).
- Enhancing Absorption: Curcumin is poorly absorbed. Pair turmeric with black pepper (piperine increases bioavailability by 2000%) and a healthy fat (like coconut oil or olive oil). Consider standardized supplements (95% curcuminoids) for therapeutic doses, under a doctor’s guidance.
- Other Notable Compounds:
- Gingerols (in Ginger): Function similarly to NSAIDs by inhibiting COX enzymes.
- Anthocyanins (in Cherries & Berries): Linked to reduced gout attacks and lower inflammatory markers.
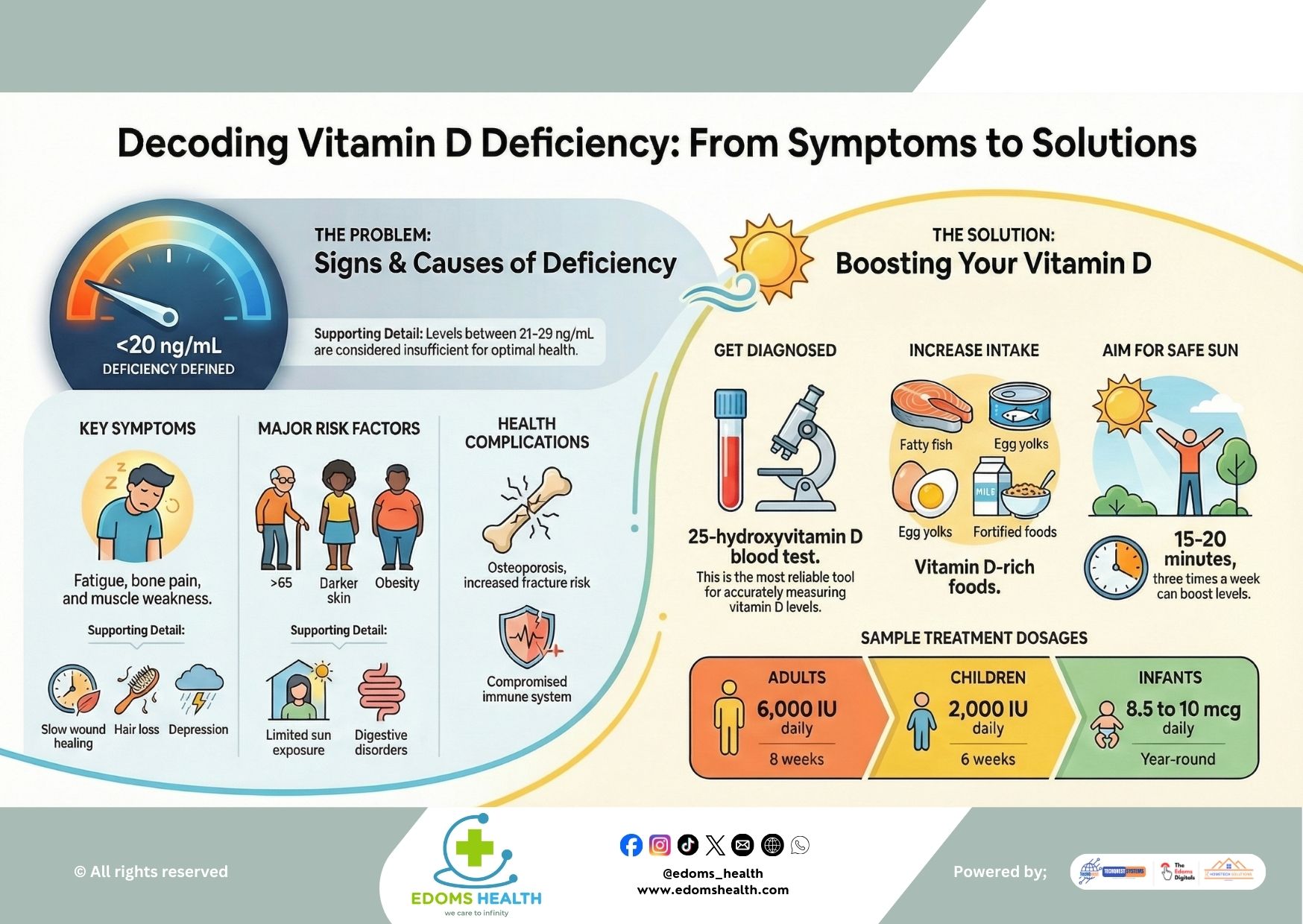
- Vitamin D: Crucial for bone health and immune modulation. Have levels checked and supplement if deficient.
Mind-Body & Adjunctive Therapies – Addressing Pain from Multiple Angles
Arthritis pain is a complex experience involving physical, neurological, and psychological components.
3.1 Manual and Physical Modalities
- Massage Therapy:
- Benefits: Reduces muscle tension that can pull on joints, improves local circulation, and may break down soft-tissue adhesions. The relaxing effect also boosts serotonin and dopamine, improving pain tolerance and mood.
- Recommended Types: Swedish massage (gentle), myofascial release, or lymphatic drainage. Communicate clearly with your therapist about pressure and sensitive areas.
- Thermotherapy (Heat & Cold):
- Heat Therapy (for Stiffness): Applying moist heat (warm towels, baths, paraffin wax) for 15-20 minutes increases blood flow, relaxes muscles, and improves elasticity of connective tissue. Ideal for morning stiffness or pre-exercise warm-up.
- Cold Therapy (for Acute Pain/Swelling): Applying ice packs (wrapped in a towel) for 10-15 minutes constricts blood vessels, reduces nerve conduction velocity, and numbs pain. Best used after activity or during inflammatory flares.
3.2 Neurological and Psychological Approaches
- Mindfulness-Based Stress Reduction (MBSR) & Meditation:
- Mechanism: Chronic pain can alter brain structure and function, amplifying pain signals. Mindfulness practice increases activity in the prefrontal cortex (involved in pain modulation) and decreases activity in the amygdala (fear/anxiety center).
- Outcome: Practitioners often report a decoupling of the sensation of pain from the emotional suffering associated with it, leading to reduced perceived intensity, less reactivity to flare-ups, and improved coping.
- Cognitive Behavioral Therapy (CBT): Effective for addressing the depression and anxiety that frequently accompany chronic arthritis, helping to change pain-related thought and behavior patterns.
Building Your Personalized Arthritis Management Plan
An integrative approach is most effective. Start slowly and build consistency.
- Assessment & Partnership: Begin by discussing these strategies with your rheumatologist or primary care doctor. Ensure they complement, rather than conflict with, your medical treatment.
- Pilot One Change Per Category: Avoid overwhelm. For example:
- Movement: Commit to a 30-minute water aerobics class once a week.
- Diet: Add turmeric and black pepper to three meals weekly, and incorporate two servings of fatty fish.
- Mind-Body: Practice a 10-minute guided meditation (using an app) each morning.
- Track and Adjust: Keep a simple journal of pain levels (0-10 scale), stiffness duration, mood, and energy. Note what helps. It provides objective data to refine your plan.
- Prioritize Sleep and Stress Management: Poor sleep and high stress are potent inflammatory triggers. They form the bedrock upon which all other strategies rest.
Conclusion: Empowerment Through Integration
Natural arthritis management is not about rejecting conventional medicine, but about embracing a broader spectrum of tools to regain agency over your health. By understanding the “why” behind the strategies—how movement protects joints, how food modulates biochemistry, and how the mind can reshape the pain experience—you can make informed, sustainable choices. This integrated, proactive approach paves the way not just for symptom relief, but for a more vibrant and engaged life.