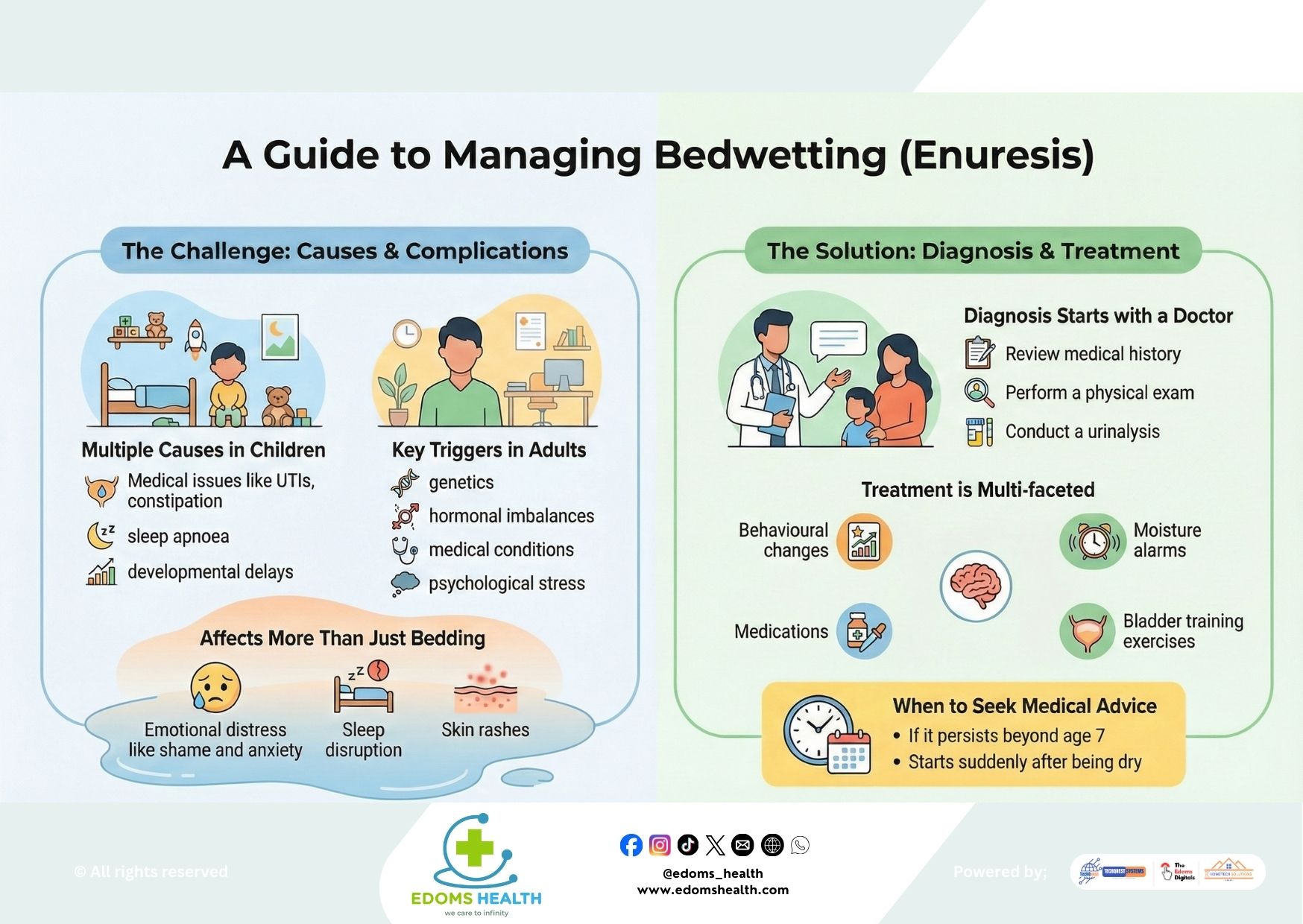
Bedwetting, medically known as enuresis, is a common condition that can affect both children and adults. While often associated with childhood, it is important to understand that bedwetting is not a behavioral problem or a sign of laziness—it is a medical issue with a variety of potential causes. With compassion, understanding, and appropriate care, most individuals can find relief and regain confidence.
Understanding Bedwetting: More Than Just an Accident
Bedwetting is defined as the involuntary release of urine during sleep in individuals who are old enough to maintain bladder control. It’s important to recognize that this condition affects emotional well-being, sleep quality, and daily life, and should be approached without blame or shame.
Common Causes in Children
In children, bedwetting is often due to a combination of factors, including:
- Delayed Bladder Maturation: The bladder may not yet have grown enough to hold urine overnight.
- Deep Sleep Patterns: Some children sleep so deeply that they don’t wake up to the sensation of a full bladder.
- Hormonal Factors: Low levels of antidiuretic hormone (ADH) at night can lead to increased urine production.
- Medical Issues: Such as urinary tract infections (UTIs), constipation, sleep apnea, or diabetes.
- Developmental or Genetic Factors: Children with developmental delays or a family history of bedwetting are more likely to experience it.
Key Triggers in Adults
When bedwetting occurs in adults, it is called secondary enuresis and often signals an underlying health concern:
- Medical Conditions: Diabetes, urinary tract infections, bladder abnormalities, neurological disorders, or prostate issues.
- Hormonal Imbalances: Similar to children, low nighttime ADH can be a factor.
- Medications: Certain drugs, such as diuretics or sedatives, may contribute.
- Psychological Stress: Anxiety, trauma, or significant life changes can sometimes trigger bedwetting.
- Genetic Predisposition: A family history may play a role.
The Emotional and Physical Impact
Bedwetting affects more than just bedding—it can take a toll on overall well-being:
- Emotional Distress: Feelings of shame, embarrassment, anxiety, or low self-esteem are common, especially in older children and adults.
- Sleep Disruption: Frequent nighttime accidents can lead to poor sleep quality and daytime fatigue.
- Skin Issues: Prolonged exposure to moisture may cause irritation or rashes.
Recognizing these impacts is an important step in offering support and seeking effective treatment.
Diagnosis: The First Step Toward Help
If bedwetting persists, a visit to a healthcare provider is essential. Diagnosis typically includes:
- Review of Medical History: Discussion of symptoms, frequency, family history, and any related health issues.
- Physical Examination: To check for signs of infection, constipation, or anatomical concerns.
- Urinalysis: To rule out infections, diabetes, or other metabolic conditions.
- Further Testing (if needed): Such as bladder ultrasounds or sleep studies, especially if other symptoms are present.
Treatment Options: A Multi-Faceted Approach
Treatment depends on the underlying cause and the age of the individual, and often involves a combination of strategies:
For Children:
- Behavioral Interventions: Encouraging regular toilet use before bed, limiting fluids in the evening, and using positive reinforcement.
- Bladder Training: Scheduled nighttime waking or exercises to increase bladder capacity.
- Moisture Alarms: Devices that sense wetness and wake the child, helping to condition a response to a full bladder.
- Medication: In some cases, desmopressin (to reduce urine production) or other medications may be prescribed.
For Adults:
- Address Underlying Conditions: Treating UTIs, diabetes, sleep apnea, or prostate issues.
- Lifestyle Adjustments: Fluid management, dietary changes, and pelvic floor exercises.
- Medications: Similar to pediatric options, tailored to adult physiology and health status.
- Therapy: Counseling or cognitive behavioral therapy (CBT) if stress or psychological factors are involved.
When to Seek Medical Advice
Consult a healthcare provider if:
- Bedwetting continues beyond age 7 in children
- It starts suddenly after a period of consistent dryness (secondary enuresis)
- It is accompanied by pain, fever, excessive thirst, or daytime wetting
- It causes significant emotional distress or impacts daily life
A Message of Support and Hope
Bedwetting is a common and treatable condition. Whether you are a parent supporting a child or an adult navigating this challenge, know that help is available and progress is possible. Open communication, patience, and professional guidance can make a meaningful difference.
If bedwetting is affecting your life or your child’s well-being, don’t hesitate to speak with a doctor. Effective management begins with understanding—and you are not alone in this journey.